Patellar Fractures - Everything You Need To Know - Dr. Nabil Ebraheim
Dr. Ebraheim’s educational animated video describes the condition of patellar fractures.
Follow me on twitter:
https://twitter.com/#!/DrEbraheim_UTMC
Patellar Fractures
Patellar fractures can involve different topic, and I am going to try and highlight the important points related to patellar fractures. The medial patellofemoral ligament is the primary stabilizer of the patella, so when the patella dislocates, you will have an injury to that ligament and also an injury to the medial patellar facet articulation cartilage or an osteochondral fragment. In addition to the medial patellar facet injury, you will get a lateral femoral condyle injury. Bipartite patella occurs in about 8% of the population. It could be bilateral in about 50%, and it usually occurs in the superolateral aspect of the patella. You should observe it and not fix it. It is not an acute fracture that may need excision or lateral retinacular release. It can occur in children between 810 years old. It is a rare condition. The patient will be unable to do straight leg raising, so you suspect that the extensor mechanism is injured. The patient may have a high riding patella on xray with a palpable gap when you examine the patient. The xray may show small flecks of bone as the patellar tendon avulses with a portion of the distal pole of the patella. Sometimes the bony injury is so small that the condition can be missed. You should have a high index of suspicion. You may need to get an MRI to confirm diagnosis. The treatment is usually ORIF if the fracture is displaced.
The patella is a large sesamoid bone. The quadriceps muscle is inserted at the proximal pole and the distal pole gives attachment to the patellar tendon. The patella is triangular in shape. The proximal 3/4 of the patella is covered with cartilage, however the distal 25% of the patella is not covered with cartilage. The patella increases the power of the extensor mechanism by about 50% because it displaces the extensor mechanism anteriorly, and that will increase the moment arm.
Transverse fractures of the patella can be nondisplaced or displaced. The patella can be pulled apart by the attached quadriceps tendon. The patient will be unable to do active extension of the knee. Upper or lower pole fractures of the patella are fractures at the site of attachment of the patellar tendon. Comminuted fractures of the patella can be nondisplaced or displaced. Comminuted fractures have multiple pieces, are very unstable, and are difficult to fix. Vertical fractures of the patella are the most common, and they are stable and nondisplaced. Osteochondral fractures of the patella are small fractures of the patella usually associated with acute dislocation of the patella.
In examination, you may feel a palpable gap. The area of the knee is usually swollen. The patient will be unable to do straight leg raise. The lateral view of the knee is the best view to see the fracture. 23 mm of displacement will probably mean that the patient will need surgery.
If you think that the patient’s extensor mechanism is intact, and the patient is able to do straight leg raise, and the fracture is nondisplaced or minimally displaced, it is usually a transverse fracture in this situation, then immobilize the knee straight in a hinged knee brace for 46 weeks with weight bearing as tolerated. Sometimes the patient cannot move the knee because of the pan and injection of lidocaine inside the knee can help to assess the integrity of the extensor mechanism. If the patient has a total knee with 2mm displacement of the patella, and the extensor mechanism is intact, then the patient will be treated conservatively in a brace or in a knee immobilizer (no surgery).
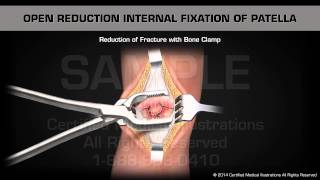
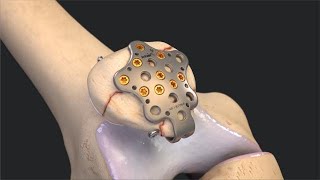
Indication for surgery is a displaced patellar fracture and the inability to do straight leg raising. First, preserve the patella (if possible). The tension band fixation technique is the gold standard. The first step in the tension band technique is to reduce the fracture with reduction clamps. Next, at least two Kwires are placed across the fracture. An anterior tension band is applied, organized in a Figure8 pattern. You need to put the Figure8 tension band wire close to the patella superiorly and not far away from the patella because that may cause construct instability and fracture displacement. A second wire may be placed circumferentially around the patella. Bending the Kwires from both ends may decrease migration of the wires and decrease the complications. The wire that is bent at both ends may be difficult to remove. Tension band fixation technique may be done with Kwires or also with cannulated screws (through the cannulated screws, you place the wires). It does not matter if you have an open or closed fracture, you treat it the same way. When you place Kwires, it means symptomatic hardware and thus a secondary reoperation. It was found that the longitudinal screws and the tension band wires are a more superior fixation.