EXTRAVASATION
/ neuralacademy
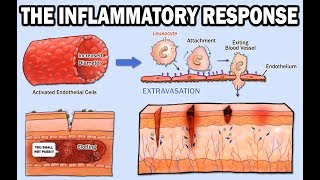
The inflammatory response is initiated within hours of infection or wounding and is triggered by physical damage to tissues or the presence of pathogens. During inflammation, there is cytokine release, vasodilation, and recruitment of leukocytes. Cytokines are substances secreted by cells of the immune system that affect other cells. Chemokines are a type of cytokine that induce directed movement of cells. Vasodilation is the dilation of blood vessels. So how do the leukocytes enter inflamed tissues?
Usually, leukocytes travel in the center of blood vessels, where blood flows the fastest. The first step of leukocyte recruitment into infected tissues is dilation of blood vessels, resulting in slower blood flow. This allows leukocytes to interact with the vascular endothelium. Now, leukocytes need to stick to the blood vessel walls.
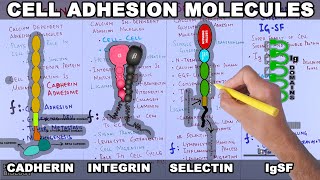
During inflammation, cytokines cause changes in the adhesion molecules on the endothelial cells, as well as the adhesion molecules expressed by leukocytes. Three kinds of adhesion molecules are important for leukocyte recruitment: Selectins, Intracellular Adhesion Molecules (or ICAMs), and Leukocyte Integrins.
Selectins are membrane glycoproteins that bind specific carbohydrate groups. They are expressed on activated endothelium and initiate endotheliumleukocyte interactions by binding to fucosylated oligosaccharide ligands on passing leukocytes. ICAMs are singlepass membrane proteins that allow for tighter adhesion of the leukocytes to the endothelium.
Leukocyte integrins are composed of two transmembrane protein chains, α and β, of which there are numerous types. Subsets of integrins have a common β chain partnered with different α chains. Leukocyte integrins important for extravasation are αLβ2 and αMβ2, which can bind to both ICAM1 and ICAM2. Integrins also allow for the convenient distinguishing of different cell types. Dendritic cells, macrophages, and monocytes feature different integrin α chains and thus display distinct β2 integrins on their surface.
Migration of leukocytes out of blood vessels extravasation. Extravasation has four steps: Rolling Adhesion, Tight Binding, Diapedesis, and Migration.
1. ROLLING ADHESION The initially weak adhesion between leukocytes and the vascular endothelium involves selectins (Pselectin and Eselectin). Pselectin appears on the endothelial cell surface within minutes of exposure to histamine, which is released by mast cells, or exposure of the endothelium to TNFα or LPS.
TNFα is a cytokine produced by macrophages upon pathogen detection and causes endothelial activation. Activated endothelial cells rapidly externalize granules called WeibelPalade bodies, which contain preformed Pselectin. TNFα and LPS also induce the synthesis of a second selectin, Eselectin, which appears on the endothelial cell surface a few hours later.
These selectins recognize the sulfated sialylLewisX moiety of certain leukocyte glycoproteins. Pselectin and Eselectin interact with these glycoproteins, allowing the leukocytes to adhere reversibly to the vessel wall, so they can “roll” along the endothelium. Without this initial weak adhesion, the stronger adhesion in the next step in extravasation can’t happen.
2. TIGHT BINDING Tight binding relies on interactions between leukocyte integrins and adhesion molecules on the endothelium, such as ICAM1 and ICAM2. Leukocyte integrins normally bind their ligands only weakly, but chemokines bound to proteoglycans on the surface of endothelial cells bind to specific chemokine receptors on the leukocyte and signal the cell to trigger a conformational change in the integrins on the rolling leukocyte, greatly increasing the adhesive abilities of the leukocyte. As a result, the leukocyte can attach firmly to the endothelium and the rolling stops.
3. DIAPEDESIS In this step, the leukocyte extravasates, or crosses, the endothelial wall. This again involves the leukocyte integrins, as well as further adhesive interactions involving an immunoglobulinrelated molecule called PECAM or CD31, expressed both on the leukocyte and at the intercellular junctions of endothelial cells. Next, the leukocyte penetrates the basement membrane with the aid of enzymes that break down extracellular matrix proteins. The movement through the basement membrane is known as diapedesis, and once the leukocyte has crossed it, it is now in the subendothelial tissues.
4. MIGRATION Migration of leukocytes through tissues occurs under the influence of chemokines produced at the site of infection. A concentration gradient of chemokines is formed along which the leukocyte can migrate to the focus of infection.
To end off, note that, even in uninfected regions of the body, circulating monocytes are continuously leaving the blood and entering tissues, where they become resident macrophages. They do so when they adhere to ICAM2, which is expressed at low levels by unactivated endothelium.